Getting tested and treated for sexually transmitted and blood-borne infections (STBBI) is important not just for a person’s own sexual health but also for preventing infections from spreading to their partners. The numbers of reportable STBBI cases are rising in Canada, with significant increases observed for syphilis and other infections over the past decade.1 Improving access to testing and treatment is a key strategy to address these trends, especially for people who commonly face barriers such as discrimination and confidentiality concerns. One approach is digital testing services for STBBI, which allow people to use websites or apps to test without needing to see a healthcare provider to get a test ordered. GetCheckedOnline, British Columbia (BC)’s decade-long digital STBBI testing program, has offered insights on how such services can benefit individuals, public health and health systems.
What is GetCheckedOnline?
GetCheckedOnline is a digital testing program for STBBI developed by the BC Centre for Disease Control (BCCDC) in partnership with the BC Public Health Laboratory, LifeLabs and regional health authorities. Launched in 2014, GetCheckedOnline is now available in nine communities across the five health regions of BC. People can get tested through GetCheckedOnline for chlamydia, gonorrhea, HIV, syphilis and/or hepatitis C. To do so, people create an account on the GetCheckedOnline.com website, fill out a sexual history questionnaire that generates a lab form and then take a printed or electronic copy of the form to a partnering lab location to provide samples. People receive an email letting them know when all of their test results have been entered into their account online. Negative results are viewed online. Positive results are discussed with a public health nurse over the phone. Follow-up care is arranged by the BCCDC’s provincial sexually transmitted infection (STI) clinic or a regional health authority partner.
What do we know about the impacts of GetCheckedOnline?
Evidence about the impacts of GetCheckedOnline is based on evaluation and research studies conducted by the Digital & Sexual Health Initiative, an applied public health research team affiliated with the BCCDC and the School of Population and Public Health, University of British Columbia. The team uses many different methods, including analysis of program data, modelling, economic analyses, surveys, interviews and focus groups. In a nutshell:
GetCheckedOnline increases the uptake of STBBI testing and treatment.
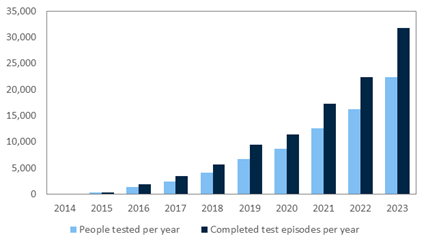
Use of GetCheckedOnline has steadily risen over time (see Graph 1), and testing conducted through this service makes up an increasing proportion of total STBBI tests in BC. In 2023, 22,344 people tested through GetCheckedOnline for a total of 31,795 completed test visits. Testing through GetCheckedOnline represented 11% of all syphilis non-prenatal tests and 8% of all HIV non-prenatal tests provincially.2
Graph 1: Uptake of GetCheckedOnline over time in British Columbia
GetCheckedOnline is valued and gives people control over STBBI testing.
People who use GetCheckedOnline report being very satisfied with the service, and they value the control they have over the testing process. As one user described3:
“I got the results within a normal time and the fact that I was able to just look it up myself and know without having to wait for a “non-call”, it was excellent. It was all-around just game-changing. I just love it.”
Male, 27 years old, gay, Vancouver
GetCheckedOnline reduces barriers people face to getting tested.
People can get tested through GetCheckedOnline without seeing a care provider, reducing many access barriers to testing in person. Studies have consistently demonstrated that GetCheckedOnline reaches people facing challenges accessing testing through healthcare providers.4–6 In a 2022 survey, 57% of people testing through GetCheckedOnline for the first time reported they had delayed, avoided or skipped STBBI testing in the past year because of barriers to accessing testing in person (e.g., needing an appointment, wait time was too long, clinic was too far away).6
GetCheckedOnline reaches people who are more likely to have an infection.
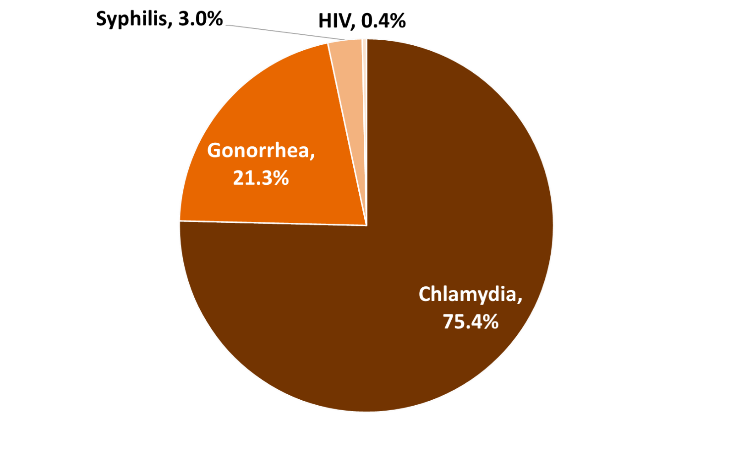
At the time of getting tested, many people are assessed through GetCheckedOnline as having risk factors for infection (e.g., condomless sex, past diagnosis of STBBI).2 This is reflected in diagnosis rates. In 2023, 6% of testing visits through GetCheckedOnline led to a positive test result. This has been fairly consistent over time. The most common diagnoses are chlamydia, followed by gonorrhea, syphilis and HIV (see Graph 2).
Graph 2: Positive results in 2023
GetCheckedOnline leads to more frequent testing, helping reduce the spread of STBBI.
Frequent testing enables early diagnosis and treatment and helps reduce further spread of infections, and research has shown GetCheckedOnline leads to more frequent testing. In an analysis of STBBI testing data between 2014 and 2017, the frequency of testing was found to be 22% higher among people who used GetCheckedOnline compared with people who tested through the BCCDC STI clinic; this discrepancy increased after the results were adjusted for characteristics associated with higher test frequency.7 In 2022, a survey of repeat users (people who got tested through GetCheckedOnline two or more times) found that four out of five repeat users said they tested earlier and more often because of the service.8
GetCheckedOnline improves the capacity of other sexual health services.
GetCheckedOnline operates as a virtual extension of the provincial STI clinic at BCCDC. As the majority of people using the service have negative results and do not need to speak with a nurse, the clinic can offer more testing overall. Over 2,000 test visits a month are completed through GetCheckedOnline with the support of a full-time nurse to manage test results; in comparison, we estimate that a full-time nurse at the provincial STI clinic performs 300 in-person test visits per month.
GetCheckedOnline reduces demands on primary care for testing.
People who use GetCheckedOnline describe using the service instead of seeing a primary care provider for testing. In the 2022 survey of repeat users, 48% reported they only tested through GetCheckedOnline, with the remainder using a mix of testing through GetCheckedOnline and providers, and 88% said they would have tested through a provider for their last test if GetCheckedOnline hadn’t been available.8
In an earlier study one user said3:
“I intend to use GetCheckedOnline all the time and I’ve already told my doctor that’s what I’m going to be doing. So he said “Fine. That’s great. That’s really good.” So I’ll go to him for my other blood work, for cholesterol and all that stuff, my overall physical. And, obviously if I did test positive for anything then I would go and see my doctor.”
Male, 62 years old, gay, Kamloops
GetCheckedOnline improves equity in accessing testing for many groups.
Some groups are more affected by STBBI and have more challenges accessing STBBI testing services. This often occurs because of social factors such as racism and the impact of historic and current colonial systems or discrimination on different aspects of identity.9,10 Our research shows that GetCheckedOnline has successfully engaged certain equity-deserving groups including youth under 30 years of age, gender and sexual minorities, and newcomers.2,8 However, work is still needed to reach other groups.
GetCheckedOnline reduces health system costs and improves sustainability.
By removing the need to see a healthcare provider to get tested, GetCheckedOnline reduces health system costs. In a 2023 economic analysis, on average, a person testing through GetCheckedOnline cost the system $38.93 less than if they had tested at a STI clinic.11 This translates into substantial cost reductions, given the high rates of testing through GetCheckedOnline.12 We estimate that GetCheckedOnline allowed BC to reduce health system costs by roughly $1.1 million in 2023.
What do these findings mean for program implementers and policy-makers?
These findings show that GetCheckedOnline has had important and positive impacts on STBBI testing in BC, which warrant its sustainment and further scale-up. More broadly, the evidence indicates that digital STBBI testing can be an effective public health strategy for STBBI management and prevention by increasing the uptake and frequency of testing and reaching people at higher risk. Leveraging technology in testing services helps to increase accessibility, particularly for people who have been historically marginalized and underserved. Potential benefits for the health system also exist because online testing can reduce demands on primary care providers and reduce health system costs.
Related resources
Digital & Sexual Health Initiative – website
Ten years later: The impacts of GetCheckedOnline – summary report
References
- Aho J, Lybeck C, Tetteh A et al. Rising syphilis rates in Canada, 2011–2020. Canada Communicable Disease Report. 2022 Feb 24;47(2-3):52-60.
- GetCheckedOnline Descriptive Report Sep. 14, 2014 – Dec. 31, 2023 (internal report). Vancouver (BC): Online Sexual Health Services, BC Centre for Disease Control; 2024.
- Knight RE, Chabot C, Carson A et al. Qualitative analysis of the experiences of gay, bisexual and other men who have sex with men who use GetCheckedOnline.com: a comprehensive internet-based diagnostic service for HIV and other STIs. Sexually Transmitted Infections. 2019 Mar 1;95(2):145-50.
- Montiel A, Ablona A, Klassen B et al. Reach of GetCheckedOnline among gay, bisexual, transgender and queer men and Two-Spirit people and correlates of use 5 years after program launch in British Columbia, Canada. Sexually Transmitted Infections. 2024 Jun 1;100(4):208–15.
- Gilbert M, Thomson K, Salway T et al. Differences in experiences of barriers to STI testing between clients of the internet-based diagnostic testing service GetCheckedOnline.com and an STI clinic in Vancouver, Canada. Sexually Transmitted Infections. 2019 Mar 1;95(2):151-6.
- Ablona A. Frequency Report GetCheckedOnline Client Experience Survey (preliminary findings). Vancouver (BC): Digital and Sexual Health Initiative, University of British Columbia, BC Centre for Disease Control; 2023.
- Gilbert M, Salway T, Haag D et al. A cohort study comparing rate of repeat testing for sexually transmitted and blood-borne infections between clients of an internet-based testing programme and of sexually transmitted infection clinics in Vancouver, Canada. Sexually Transmitted Infections. 2019 Nov 1;95(7):540-6.
- Gilbert M, Ablona A, Iyamu I et al. Online and provider-based testing for sexually-transmitted and blood-borne infections: describing patterns of use among repeat testers in British Columbia, Canada. In: STI & HIV World Congress 2023, Chicago, Illinois, July 24–27, 2023. Available from: https://dishiresearch.ca/resource/online-and-provider-based-testing-for-stbbis/
- Stewart M, Ryu H, Blaque E et al. Cisnormativity as a structural barrier to STI testing for trans masculine, two-spirit, and non-binary people who are gay, bisexual, or have sex with men. PLoS ONE. 2022 Nov 28;17(11):e0277315.
- Dulai J, Hassan A, Stewart M et al. Perspectives on digital testing services for sexually transmitted and blood-borne infections from Two-Spirit, gay, bisexual, transgender, and other queer Black, Indigenous, people of colour living in Ontario, Canada. Ethnicity & Health. 2024;29(4–5):533-52.
- Krueger H. Economic analysis of British Columbia's GetCheckedOnline Program: cost per course of screening and diagnosis (preliminary draft). Delta (BC): H. Krueger & Associates Inc.; 2023 May.
- Allan L. Cost analysis of BC Centre for Disease Control’s (BCCDC) two sexually-transmitted and blood-borne infection (STBBI) screening programs (unpublished report). 2019 Aug.
About the author(s)
Hsiu-Ju Chang is a research manager supporting the Digital & Sexual Health Initiative and other researchers in the Clinical Prevention Services at the BCCDC. She supports projects in the areas of sexually transmitted and blood borne infections, tuberculosis and digital public health, with a strong focus on equity.
Mark Gilbert is a public health physician of the BCCDC and an associate professor at the University of British Columbia School of Population & Public Health. Mark is the medical lead for the Online Sexual Health Services program at BCCDC and conducts research to support the development of internet-based approaches to sexual health service delivery, including BC's sexual health education website SmartSexResource and internet-based STBBI testing program GetCheckedOnline. Mark also leads the research program Digital & Sexual Health Initiative, and holds an applied public health chair related to improving sexually transmitted and blood borne infection testing systems.

